Medical policy and clinical guidelines
Genetic testing requests are evaluated against evidence-based clinical appropriateness guidelines and/or health plan medical policy, as required by each patient’s health plan.
Clinical guideline development process
Carelon Medical Benefits Management will first apply any clinical criteria from the health plan, whether in the form of medical policy or clinical guidelines. In the event that the health plan does not have applicable clinical criteria, Carelon uses clinical appropriateness guidelines that are based on established, evidence-based criteria and developed in consultation with panels of academic thought leaders and community physicians from across the country. The process for assessing the clinical appropriateness of testing is consistent with the CDC ACCE Model Process for Evaluating Genetic Tests. Guidelines are formally reviewed and updated annually but may also be updated more frequently as needed based on the publication of new literature or supporting evidence. Our panelists meet and review evidence quarterly.
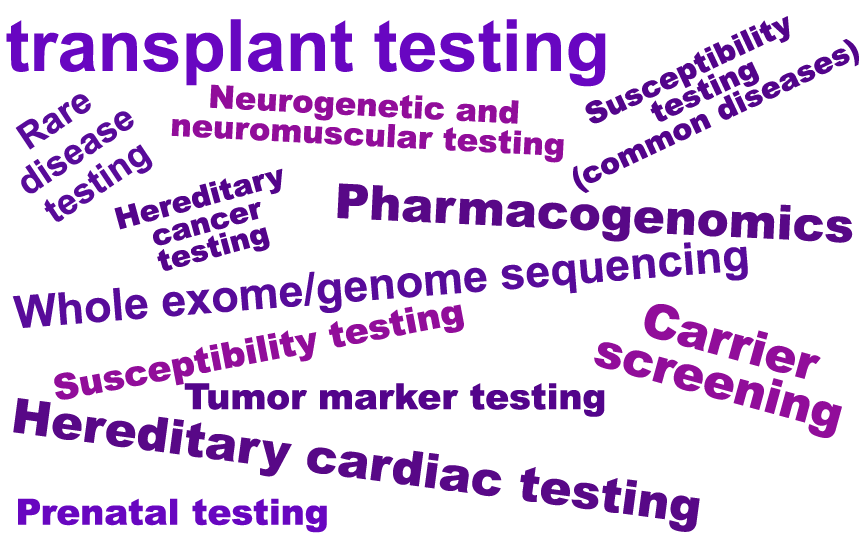
Genetic testing requests may be submitted by providers with varying medical specialties. The categories of genetic testing and medical specialties impacted by the program may vary from health plan to health plan.
Program designs vary by health plan. We encourage you to review the FAQs for each patient’s plan on the Resources page.