All Solution Tips and Tricks
All of our provider microsite links are posted on the Carelon provider portal, but did you know that our Provider Connections news blog is accessible from each solution’s microsite? Microsites are mini websites that give information about Carelon solutions, such as Radiation Oncology. You can access the News blog site to see our current and past issues of Provider Connections.

Carelon MBM Program Reminders
To help ensure adherence to evidence-based medical policies and clinical guidelines, a minimal subset of prior authorization requests is subject to an existing Carelon MBM audit process.
If your request has been selected for an audit, you will be prompted to submit additional clinical documentation and/or participate in a peer-to-peer consultation with a Carelon physician reviewer. We kindly ask that you complete these requests in a timely manner, as this will help expedite the audit and decision processes.
Evidence assessment:
Did you know that the Carelon MBM Guideline Development team conducts a systematic evidence review to inform both new guidelines and annual updates? A key component of the process is an assessment of the collected evidence by a trained methodologist using standardized tools such as Quality Assessment of Diagnostic Accuracy Studies (QUADAS), Standards for Reporting of Diagnostic Accuracy (STARD), Diagnostic Accuracy Quality Scale (DAQS), and the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE).
These tools provide a systematic way to determine whether a particular article meets the standard of quality needed to inform clinical decision-making. They take into account such factors as bias, the size and composition of the study group, and the statistical methods used to evaluate the findings.
For more information on our evidentiary review process, visit our Clinical Guidelines and Pathways page, clinical guidelines access section: https://guidelines.carelonmedicalbenefitsmanagement.com/
Did you know?
Available 24/7, each of our MBM solution microsites include valuable resources for you and your peers.
Visit our Resource pages to learn more about our programs and access helpful information and tools including:
- Order entry checklists
- Clinical guidelines
- Direct access to our MBM provider portal and clinical guidelines
- FAQs and more
Updates are applied to our solution microsites frequently, so we encourage you to visit them often to ensure you have the latest program information available.
For easy future reference, be sure to bookmark the Resources page/s that match your specialty.
MBM solution provider microsite Resources links:
- Radiology provider website: https://providers.carelonmedicalbenefitsmanagement.com/radiology/
- Cardiovascular provider website: https://providers.carelonmedicalbenefitsmanagement.com/cardiovascular/
- Sleep provider website: https://providers.carelonmedicalbenefitsmanagement.com/sleep/
- Musculoskeletal provider website: https://providers.carelonmedicalbenefitsmanagement.com/musculoskeletal/
- Rehabilitation provider website: https://providers.carelonmedicalbenefitsmanagement.com/rehabilitation/
- Genetic Testing provider website: https://providers.carelonmedicalbenefitsmanagement.com/genetictesting/
- Radiation Oncology provider website: https://providers.carelonmedicalbenefitsmanagement.com/radoncology/
- Medical Oncology provider website: https://providers.carelonmedicalbenefitsmanagement.com/medicaloncology/
- Surgical provider website:
https://providers.carelonmedicalbenefitsmanagement.com/surgicalprocedures/
Have you visited our Carelon Medical Benefits Management website recently? Check out the latest updates for providers.
Another great complimentary resource you may want to bookmark is our Carelon Medical Benefits Management website for continued easy access to our provider portal and tools, new program information, important program enhancements, training opportunity news, access to our Provider Connections news blog and more: https://www.careloninsights.com/medical-benefits-management/specialty-care
There is a convenient Providers drop down menu in the navigation bar that provides quick access to such tools as:
- Carelon MBM clinical appropriateness guidelines and pathways*
- Our provider resources access page
- Carelon MBM provider portal
*From our clinical appropriateness guidelines and cancer treatment pathways page, you can now conveniently toggle between our Provider Connections blog page and the guidelines page.

Direct access to Carelon Post Acute Solutions program info and provider resources
Through our post acute care programs, we ensure patients receive quality, seamless care when and where they need it most, such as the home or a post-acute care facility..
We do this by working with providers like you or our own local network to align care with the latest evidence and health plan care management plans.
If you service post-acute solutions members, you’ll also find convenient access from our Providers drop down menu to:
Solution-specific tips you can use
Visit the Additional Outpatient UM provider microsite to access helpful information and tools such as a direct link to the provider portal, clinical guidelines, FAQs and more.
Visit the Back Pain Program provider microsite to access helpful information and tools such as a direct link to the provider portal, clinical guidelines, FAQs and more.
Reminder: Imaging & Management of Low Back Pain provider video now available within MBM provider portal*
Do you ever question the need for imaging when a patient complains of low back pain, or wonder what imaging or treatments to start with? In this short 15-minute video on Imaging & Management of Low Back Pain, we discuss the etiologies of low back pain, clarify the role of imaging and associated harms/risks, and review current evidence-based treatment recommendations.
To access this video, please go to the Provider Portal® home page and login then navigate to the Help Center > Provider Webinars > All Solutions section. Finally, click on “Imaging & Management of Low Back Pain Training” to watch the video. Once you have completed the video, please complete this survey link to help us determine if the video was helpful. Your feedback* helps our content development in the future.
You can also access the training video on our blog page here.
*Survey feedback and participation may be shared with your health plan.
Visit the Cardiovascular provider microsite to access helpful information and tools such as a direct link to the provider portal, clinical guidelines, FAQs and more.
Reminder: Our Cardiology Solution will be renamed to Cardiovascular Solution effective this July
If you work with our Cardiology Solution, please note that over the next two months you will notice a name change being applied wherever referenced. The new name, Cardiovascular Solution, is being applied in our MBM provider portal, training materials, and other documentation. Our provider microsite name and URL have also been updated to include the new Cardiovascular name: https://providers.carelonmedicalbenefitsmanagement.com/cardiovascular/.
Our health plan clients often use customized names for their programs with us. They’re permitted to select the best program name that works for them, so you may continue to see some usage of Cardiology Program on health plan websites.
Reminder notices will remain programmed on our Provider Connections blog and on our Cardiology provider microsite through close out of the name transition.
Visit the Genetic Testing provider microsite to access helpful information and tools such as a direct link to the provider portal, clinical guidelines, FAQs and more.
Harvard Pilgrim providers: Please visit the Harvard Pilgrim Genetic Testing provider microsite.
Genetic Testing Program Updates Coming this February
Effective February 8th, requests for the Carelon MBM Genetic Testing Program will no longer hard stop users if the date of service does not match the date of collection. While the date of service is still defined as the sample collection or retrieval date in alignment with CMS policy, this policy does allow for a number of exceptions. This enhancement is expected to better support these exceptions.
For health plans that previously enforced this date match in alignment with our updated definition, the valid timeframe for authorizations will begin with the date of service provided.
For questions, please contact the genetic testing solution team at genetictestingsolution@carelon.com.
Our Genetic Testing Program email address has changed
If you work with our Genetic Testing Program and need to email us, please note that our program email address has changed from DL-genetictestingsolution@carelon.com to genetictestingsolution@carelon.com.
For your convenience, our email address can also be found on our program microsite and Provider Connections blog site ongoing.
Our provider microsites provide access to helpful information and tools such as a direct link to the provider portal, clinical guidelines, FAQs and more. Contact your health plan representative for the program link applicable for their Carelon Medical Oncology program.
2025 in Oncology Therapeutics:
Targeted Agents, ADCs, and the Cost-of-Care Implications
In 2025, oncology again led FDA therapeutic-area activity, underscoring why oncology remains a primary driver of health plan specialty spend and operational complexity. There were 54 oncology-related FDA actions across the year, spanning not only new approvals but also supplemental indications, conversions, and formulation/biosimilar events—each of which can influence utilization patterns and downstream total cost of care.
From a “new drug” perspective, FDA/CDER reported 46 new drugs approved in 2025, and 16 (35%) were oncology agents that were novel-to-market therapeutic products and select novel formulations.
While small molecules predominated—particularly biomarker-defined targeted agents—the modality mix also included two antibody–drug conjugates (ADCs), one BCMA×CD3 bispecific T-cell engager for multiple myeloma. There were 14 new indications for immune checkpoint inhibitor (ICI) drugs, three of which were for pembrolizumab (Keytruda) specifically. And there was also approval in September 2025 (earlier than expected) of the subcutaneous-enabling pembrolizumab formulation (pembrolizumab and berahyaluronidase alfa-pmph; Keytruda QLEX)
There is continued acceleration of biomarker-defined solid tumor care, where therapy selection is tightly coupled to testing strategy, specimen adequacy, and line-of-therapy decisions. Non–small cell lung cancer (NSCLC) is the most concentrated example, with multiple new targeted entrants keyed to ROS1, EGFR exon 20, HER2 activating mutations, and high c-Met protein overexpression. Breast cancer also features prominently, including an ESR1-mutated ER+ / HER2− targeted therapy and an ADC for HR+ / HER2− disease. This is not merely a drug-management issue; it is a molecular diagnostics management issue. Effective utilization management (UM) is essential in medical oncology treatment and genetic testing and requires increasing sophistication to embed biomarker gating and line-of-therapy criteria directly into prior authorization to reduce off-label drift and also ensure that testing (tissue and/or ctDNA) is appropriately aligned with treatment intent.
Finally, drug spend will continue to skew toward infused/clinic-administered specialty therapies (ADCs, bispecifics, immune checkpoint inhibitors and other biologics). The fact that there are now seven systemic anti-cancer therapy biologics with subcutaneous delivery options may shift some aspects of care delivery and workflow mechanics for providers, but this should not be assumed to automatically reduce gross drug spend.
Oncology’s New Cost Curve: What ASH & SABCS 2025 Mean for Health Plans
The 2025 American Society of Hematology (ASH/hematology) and San Antonio Breast Cancer Symposium (SABCS/breast cancer) meetings held in December delivered a clear message for payers: oncology is shifting toward highly targeted, often time-limited treatments that reduce reliance on traditional chemotherapy but drive higher up-front spending on drugs and diagnostics. For health plans of all types, the business question is how to prepare benefit design, utilization management, and network strategy for 2026.
In breast cancer, powerful antibody-drug conjugates (ADCs) and new oral targeted agents are moving earlier in the care pathway. Therapies once reserved for metastatic “salvage” use are now being used in curative settings and in the first or second line for advanced disease. Early-stage hormone receptor–positive disease is migrating from inexpensive generic endocrine therapy toward branded oral endocrine agents and CDK4/6 inhibitor combinations used for years. HER2-positive patients are more likely to receive ADCs in place of, or in addition to, conventional chemotherapy. For plans, that means larger patient cohorts exposed to high-cost agents and more complex monitoring for toxicities, even as hospitalization for traditional chemo complications may gradually decline.
In hematologic malignancies, bispecific antibodies and next-generation targeted drugs are reshaping treatment algorithms. In multiple myeloma and follicular lymphoma, bispecifics are shifting from late salvage to earlier relapse, often in fixed-duration regimens. These drugs require specialized centers and close early monitoring but can produce deep remissions and defer later intensive therapies such as transplant or CAR-T. In chronic lymphocytic leukemia (CLL) and chronic myeloid leukemia (CML), new evidence supports finite-course targeted combinations and structured treatment discontinuation strategies, replacing the historic “pay forever” model of continuous oral therapy. This front-loads cost but offers the prospect of lower lifetime drug spend if patients can safely stop treatment.
A cross-cutting theme is the rising role of advanced diagnostics. Blood-based circulating tumor DNA and minimal residual disease tests are increasingly used to decide when to start, switch, or stop therapy. These assays are not incidental—they represent a recurring cost that must be tied to clear, evidence-based management decisions.
For health plans, 2026 will bring sustained upward pressure on pharmacy and lab budgets. The strategic response is not simply restriction, but precision: disease- and line-specific prior authorization; preference for time-limited regimens when outcomes are comparable; concentration of high-acuity therapies in capable centers; and robust outcomes analytics to determine whether higher up-front spend is being offset by fewer hospitalizations, less salvage therapy, and better long-term control of disease.
Optimizing Immunotherapy: A 24-Month Planned Discontinuation Strategy for Advanced Solid Tumors
As more patients with advanced solid tumors experience sustained benefits from immune checkpoint inhibitors (ICIs), discussions about the optimal duration of therapy have become increasingly important. Current guidelines, combined with clinical evidence, now support considering a planned discontinuation strategy after 24 months for selected patients who have achieved and maintained disease control. This approach seeks to minimize cumulative toxicity, reduce treatment burden, and manage healthcare resources effectively without compromising patient outcomes.
The evidence for a 24-month discontinuation strategy is built on early pivotal trials that typically limited ICI therapy to two years. Long-term follow-up data from these trials indicate that many patients maintain durable responses post-therapy. A number of observational studies also support this strategy. For instance, a study by Sun and colleagues published in JAMA Oncology demonstrated no significant difference in overall survival between patients undergoing a fixed two-year ICI course and those on indefinite therapy, suggesting no additional survival benefits from prolonged treatment for controlled cases. In addition, a systematic review and meta-analysis called the OTHERS study, which analyzed data from 57 trials involving over 22,000 patients with solid tumors, further affirmed that a two-year ICI treatment combined with standard care improved overall survival outcomes in patients with non-small cell lung cancer (NSCLC) compared to extended ICI treatment duration.
Regarding current guidelines, the NCCN and FDA label endorse a two-year maintenance duration of ICI therapy for NSCLC patients who have not shown progression following first-line immunotherapy. ASCO-endorsed clinical evidence also supports considering immune checkpoint inhibitor treatment discontinuation after 24 months in progression-free patients with selected solid tumors. In addition, SITC consensus documents acknowledge this timeframe as standard in clinical trials.
To implement the 24-month stop effectively, care providers should select patients who have not shown disease progression after frontline immunotherapy for several advanced solid tumors, including NSCLC, head and neck squamous cell cancer, and others like colorectal cancer, Hodgkin lymphoma, cervical cancer, and certain others. Monitoring post-discontinuation should involve close surveillance using standard imaging techniques. Currently, there’s no validated biomarker available to guide these decisions, although research is ongoing.
If disease progression occurs following therapy discontinuation, a rechallenge with PD-1/PD-L1 blockade is feasible, though efficacy may be reduced compared to initial treatment. Providers should discuss expectations and potential outcomes with patients upfront.
In summary, considering the toxicity and costs associated with ICIs, a planned discontinuation at 24 months can significantly reduce financial burdens on patients and the healthcare system without compromising therapeutic outcomes. This approach is supported by both trial data and real-world evidence, indicating that many patients maintain long-term progression-free and overall survival after stopping treatment at the two-year mark.
Accessing our Cancer Treatment Pathways and Guidelines:
To view our Carelon Cancer Treatment Pathways and Guidelines, visit https://guidelines.carelonmedicalbenefitsmanagement.com/current-cancer-treatment-pathways-guidelines/.
References:
- Bogani G, Cinquini M, Signorelli D, et al. A systematic review and meta-analysis on the optimal treatment duration of checkpoint inhibitoRS in solid tumors: The OTHERS study. Crit Rev Oncol Hematol 2023, PMID # 37156405
- Bozorgmehr M, Muller A, Rawluk J, et al. Immune checkpoint inhibitors in non-small cell lung cancer – When should we dare to stop treatment? Lung Cancer 2023, PMID # 37657237
- National Comprehensive Cancer Network. Non–Small Cell Lung Cancer Clinical Practice Guidelines, v1.2026, NSCL-K
- Nivolumab FDA label, April 2025
- Pembrolizumab FDA label, May 2025
- Sun L, Beliberg B, Hwant WT, et al. Association between duration of immunotherapy and overall survival in advanced non-small cell lung cancer. JAMA Oncol 2023; PMID # 37270700
Carelon Medical Oncology Program drug entry – regimen abbreviation list now available on provider microsite
For your convenience, our Medical Oncology team has prepared a new Regimen Abbreviation document that can assist with the drug entry on process on the Requested Services screen.
You can find it under our Resources page here.

Additional Medical Oncology Program documents we have posted for easy reference for you and your practice include:
-
- Program overview
- Quick guide to order entry
- How to register for provider portal
- Steps to get your practice ready checklist
- How to submit a pathway inquiry
Be sure to bookmark our Medical Oncology provider microsite Resources page for future reference.
Archived articles
View past Medical Oncology Tips articles here.
Visit the Musculoskeletal provider microsite to access helpful information and tools such as a direct link to the provider portal, clinical guidelines, FAQs and more.
What’s new in the Musculoskeletal Program?
Our dedicated Musculoskeletal Program team has prepared some helpful tips and updates for you and your team members.
New enhanced functionality:
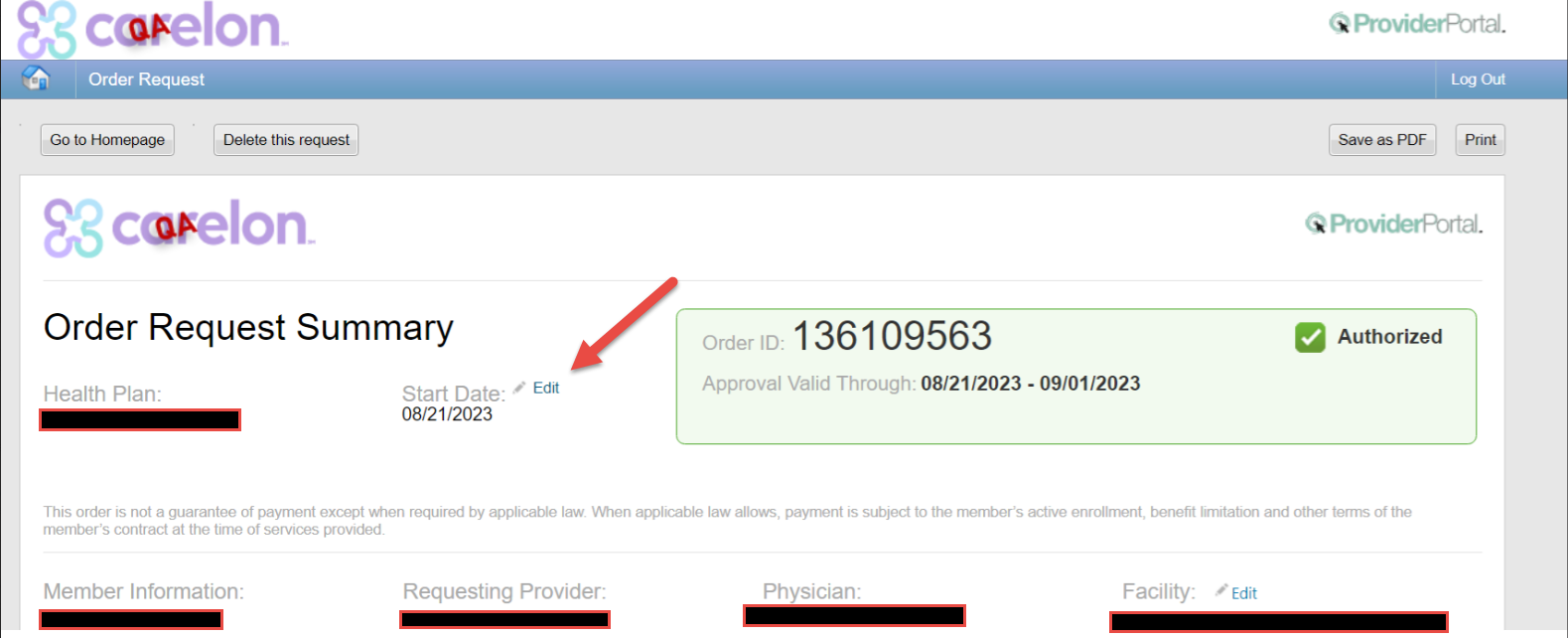
Our Musculoskeletal Program now allows the date of service to be changed on our provider portal for approved prior authorizations. We recognize that surgical dates can change and wanted to make it easier for providers to make this update without having to call Carelon.
Tip #1: The top five critical ingredients we need you to send to help authorize your case are:
-
- Your physician’s note needs to describe the exact surgery being planned, and the reason the surgery is needed.
- The note needs to say when the patient started having pain/symptoms, the severity of the pain, and how the pain effects the patient’s activities.
- The note needs to include an assessment of the physician’s recent exam of the painful area.
- The note needs to tell us what type of treatment the physician prescribed, how long the patient tried the treatment, and if the treatment improved the patient’s pain/symptoms.
- A copy should be sent of the radiologist’s report of any recent x-ray, CT, MRI, or ultrasound ordered by the physician to diagnose the reason for the pain/symptoms.
If any of these are missing, we may not have enough information to authorize your case.
Note: For a procedure to be pre-authorized, the notes have to show that your patient has the symptoms, exam, treatment, and imaging that meet Carelon’s criteria for the surgical procedure you are requesting. You can view the criteria at: (put in link for Joint guidelines).
Tip #2: Did you know that some procedures must have a radiologist report for pre-authorization?
If your doctor ordered a CT scan or MRI to find out the reason your patient has pain/symptoms, you need to send us a copy of the radiologist’s report.
Some offices copy and paste the report’s “impression” into their Electronic Medical Record (EMR). The impression does not always include important information that is in the rest of the report.
To avoid delays with your authorization request, remember to submit the radiologist’s report.
Providers can check the microsite for 2023/2024 quarterly session dates and sign-up for a future training session on our Musculoskeletal Program microsite.
Visit the post-acute provider microsite to access helpful information and tools such as a direct link to the provider portal, provider materials, program information and more.
Post-Acute Complete: Turning the post-discharge window into wins
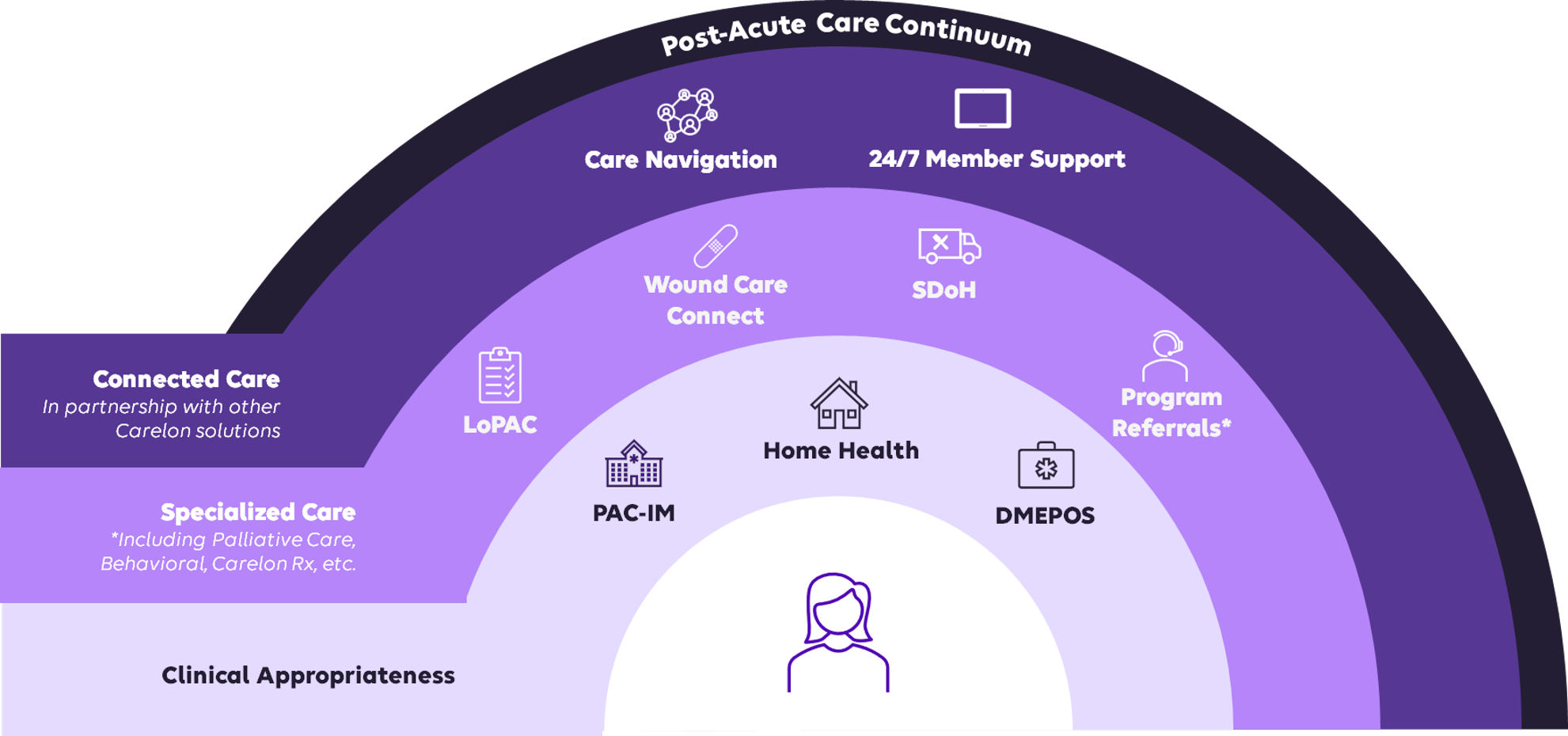
When patients leave the hospital, minutes matter. Post-Acute Complete connects care coordination, personalized clinical support, and proactive transition planning to directly improve patient outcomes and reduce unnecessary costs. It consists of several turnkey solutions that simplify complex transitions for a seamless patient and care provider experience.
Care Navigation and Wound Care Connect (WCC) are two solutions that provide tighter post-discharge follow-through, moving the needle on engagement, readmissions, utilization, and cost.
Driving better outcomes and improved coordination with Care Navigation:
Our Care Navigation program helps members manage their health journey by guiding them through the complex healthcare system and connecting them with the right services at the right time. Members are assigned to a Care Navigator who assists them with identifying appropriate community-based services, scheduling follow-ups, understanding benefits, and overcoming barriers to care—ensuring smoother transitions and better outcomes.
- More connection with fewer bounce-backs. Members enrolled in Care Navigation showed an eight-point engagement lift within 30 days post-discharge and a 16.5% reduction in observed-to-expected readmission ratio1.
- Admissions trending down. After discharge, inpatient admits fell across settings: -18% in medical settings, -40% in non-acute settings, and -58% for behavioral health1.
- Meaningful cost impact. Enrolled members saw impactable savings: an 11% total cost decrease, including a 24% reduction in avoidable medical expenses1.
Wound care, simplified
Wound Care Connect (WCC) provides enhanced services to members with complex wounds and ostomies, including timely access to wound care specialists, digital wound monitoring, and care coordination. Certified wound and ostomy nurses partner with your patients’ at-home care team to consult on optimal care pathways and closely monitor wound progression and healing.
Active WCC participants had zero wound-related inpatient admits2 during participation. After discharge, wound-related ER use dropped and discharged patients consistently showed lower or comparable ER and inpatient utilization over time2.
What you and your practice can expect
As members approach discharge, Carelon Care Navigators will be ready and prepared to coordinate resources to prevent readmission and identify any gaps in the discharge plan. A Care Navigator may reach out to members, their caregivers, or your facility’s discharge planner to coordinate care efforts.
To see if your patients with wounds or ostomies may qualify for Wound Care Connect, talk to the assigned Care Navigator or contact your Carelon provider services representative.
Why this matters
These results point to a simple story: when post-acute support is structured and proactive, patients stay engaged, avoid unnecessary admits, and total cost curves start to bend. Carelon’s Post-Acute Complete provides that structured support so that you can focus on what matters most: providing the best care possible to your patients.
Contact your Carelon provider services representative today to ensure your patients have access to coordinated, personalized care.
1 Internal data, March 2022- September 2023. CTI (Care Transitions Intervention) was evaluated across 14,220 Medicare members.
2 Internal WCC outcomes data, November 2022 – September 2023
Home Health Program NOMNC Education Reminder
As a reminder, ensuring the correct process is followed when submitting the Notice of Medicare Non-Coverage (NOMNC) is important. Per CMS guidelines, the NOMNC must be provided to the member at least two calendar days before Medicare-covered services end. A reduction in services does not require the NOMNC to be issued at that time. However, it must still be delivered in accordance with CMS requirements and before the final discipline is discharged.
Once all home health services have ended, please upload the NOMNC to the Carelon portal so we can issue the DENC no later than the close of business on the day the QIO provides notification, as required by regulation.
The NOMNC contains the appeal rights for the member, so it will be required when a member files an appeal. Included on the document should be the due date, member or member representative’s signature, and the date it is signed. Please ensure these elements are present when submitting.
To support ongoing compliance with the CMS NOMNC requirements, we will continue to review this process. Should any areas of non-compliance be identified, we will partner with your agency to create a corrective action plan that supports compliance and strengthens our shared commitment to quality and regulatory standards.
Effective December 1, 2025, Carelon discontinued sending blank NOMNC forms when a partial or full denial is issued. If you need a blank NOMNC form, you can access it through our provider portal or directly from CMS at the link below.
Additional information is available on the CMS website: CMS NOMNC
We appreciate your continued partnership!
If you have any questions, please contact the Provider Relations team via email at HHProvider_Relations@Carelon.com.
Stay Informed: Carelon MBM Post-Acute Updates & Reminders
CMS Regulation Changes Effective 2026 – As part of our ongoing commitment to regulatory compliance and service excellence, Carelon MBM thoroughly reviewed the 2026 CMS regulation guideline changes. We are pleased to confirm that all of our operational practices are fully aligned with these upcoming requirements.
Key Update Effective January 1, 2026
CMS requires a reduction in turnaround time from 14 calendar days to 7 calendar days for standard requests received on/or after January 1, 2026. We recognize the importance of this change and have actively enhanced our internal processes to ensure we meet the new 7-day turnaround standard by the effective date.
If you would like to review the official CMS guideline changes, please refer to the following link: 2026 CMS Policy Changes.
2025 Carelon Provider Survey – Our 2025 Carelon PAS Provider Survey was sent out November 11th. Your feedback matters! Please complete the provider survey to help us improve our services and support. The survey closes this Friday, November 21st.
Visit the Radiation Oncology provider microsite to access helpful information and tools such as a direct link to the provider portal, clinical guidelines, FAQs and more.
Archived articles
View past Radiation Oncology Tips articles here.
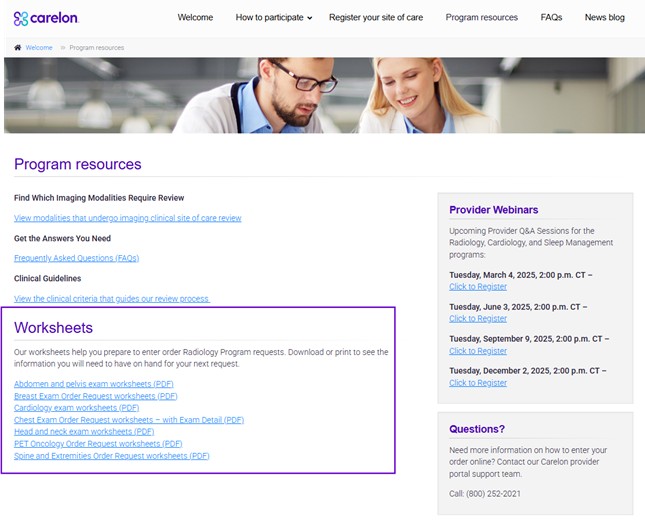
Visit the Radiology provider microsite to access helpful information and tools such as a direct link to the provider portal, clinical guidelines, FAQs and more.
Now available: Updated Radiology Program Order Request Checklists
Knowing what information, you will need for each order saves time. Our order request checklists, also referred to as clinical worksheets, can help you and your peers identify and collect the information you need to have available when entering an order request.
We recommend that you print a copy or save it to your computer to refer to when you are preparing to submit an order. You can also bookmark our Resources page for easy future reference.
Our recently updated Radiology Program clinical worksheets are available on the Resources page of our Radiology provider site.
Options include:
- Abdomen and pelvis exam worksheets (PDF)
- Breast Exam Order Request worksheets (PDF)
- Cardiology exam worksheets (PDF)
- Chest Exam Order Request worksheets – with Exam Detail (PDF)
- Head and neck exam worksheets (PDF)
- PET Oncology Order Request worksheets (PDF)
- Spine and Extremities Order Request worksheets (PDF)
Don’t wait. Register your imaging site of care with OptiNet today!
Carelon understands the key role that medical practices play in the delivery of care for patients who require imaging studies. Developed in collaboration with health plans, our Radiology Program helps support quality care that is consistent with current medical evidence and delivered in the most clinically appropriate setting.
Our program includes OptiNet, which is available in the provider portal. OptiNet is a proprietary, multifaceted program designed to collect service and capability information on outpatient imaging providers.
About OptiNet
Available to our health plan clients, OptiNet is the Carelon assessment tool that gives providers more transparency when ordering high-tech imaging procedures and more. OptiNet generates a modality score based on equipment, staffing, and quality control information reported by the facility.
It is available in the provider portal.
Register your imaging facility today!
Choosing an imaging provider is an important decision for our customers, affecting the quality and cost of their care. The Carelon OptiNet tool will help providers and their patients compare high value, lower cost imaging facilities for computed tomography (CT) imaging, magnetic resonance (MRI) imaging, and other imaging services.
Why is registration important?
When you register, your facility information is displayed in the provider portal. By registering, your facility may be available on our Initial Display List to ordering physicians and members requesting imaging services. Providers register sites within OptiNet to become eligible alternate sites for our Site of Care and Carelon Specialty Care Shopper (member engagement) programs.
What do you need to do?
Register in the OptiNet tool.
How to register
- Log in to the provider portal at https://providerportal.com.
- Select “Access Your OptiNet Registration” found on the left-hand side of the provider portal home page.
- OptiNet will guide you through the registration process.
What data will be included?
The Carelon online registration tool, OptiNet collects data on imaging providers related to facility specifications, technologist and physician qualifications, accreditation, equipment features, and technical registration. This information is used to determine how organizations conform to industry-recognized standards, including those established by the American College of Radiology (ACR) and the Intersocietal Accreditation Commission (IAC).
For more Information:
View our provider microsite to learn about the many benefits of OptiNet.
If you have any questions about the OptiNet registration or score card generation, please contact the Carelon Assessment Department at 877.202.6543 or by email at Assessment@aimspecialtyhealth.com.
Visit the Rehabilitation provider microsite to access helpful information and tools such as a direct link to the provider portal, clinical guidelines, FAQs and more.
Rehabilitation program tips
Rehabilitation providers: For easy reference, here is a summary of recent information added to our FAQs posted on the rehabilitation microsite.
Rehabilitation program updates: What’s new at Carelon Medical Benefits Management?
We have implemented some enhancements to our Carelon MBM Rehabilitation program that we’re excited to share with you!
We recently updated the Rehabilitation provider search functionality within therapy requests. Previously, users were asked to name the billing entity, and if applicable, were also asked to enter the treating therapist for the request. Following the update, users are only being asked to enter the provider who is selected as the billing entity for the request.
The Rehabilitation program recently completed a clean-up of therapy requests that had been initiated by a portal user, but not submitted. Carelon canceled out any incomplete requests that were open for more than seven days.
If the user pulls up one of the canceled requests, they will get a message letting them know it was canceled due to being open for more than seven days, “This request was canceled due to being open more than seven days. If the service is still needed, please start a new request.” If skilled services are still required, the user will need to submit a new request.
How often should providers update the episode of care initial evaluation date in the Carelon portal for members receiving long-term therapy services?
Within the Carelon rehabilitation program, requests are staged based on the initial evaluation date of service as well as the previous request for medical necessity determination. For these reasons, providers are asked to keep the initial evaluation date consistent throughout the member’s episode of care when submitting prior authorization requests for additional treatment.
There is one scenario in which the initial evaluation date may change and that is typically for chronic, long term or pediatric episodes of care that extend past a calendar year of treatment. In these scenarios, there is a reasonable expectation that the initial evaluation and plan of care would be updated annually. The updated initial evaluation date should also be documented annually within in the member’s therapy treatment requests on the Carelon portal.
What should a provider do if they have not received the request determination, but the patient is scheduled to return for treatment soon?
If a provider has not received a determination on their request and the patient is returning to the facility, the provider may contact the Carelon Call Center and ask that the request be reviewed live. If the provider is unable to hold while the request is reviewed, the provider facility can request a call back once the review is completed.
What are the most common reasons a second treatment prior authorization request receives a lower visit allocation (i.e., 2-4 visits)?
When a second treatment request received a lower than typical visit allocation, there are a few possible reasons for this outcome.
-
-
- Did the provider document an in-scope functional outcome tool (from the microsite list) on the initial treatment request and document a baseline score?
- Did the provider reference the scoring scale on the provider microsite to ensure that the functional outcome tool score documented matched the scoring scale that Carelon utilizes?
- Did the provider document an in-scope functional outcome tool (from the microsite list) on the second treatment request and document an updated score from the member’s most recent visit?
- Did the provider document a mitigating factor in the event of little to no progression documented on the functional outcome tool score between the initial or second treatment requests?
- Did the provider document a change to the plan of care in the event of little to no progression documented on the functional outcome tool score between the initial or second treatment requests?
- Did the provider document short-term goal achievement on the second treatment request?
- Has a benefit limit been reached, where benefit limits apply?
- Has the member achieved the plan of care functional goals when two visits may be appropriate for discharge planning and home exercise program instruction?
-
The provider has the option to call Carelon at any time for a peer-to-peer discussion if they feel the details of their request need to be clarified.
To access our full set of rehabilitation program FAQs, visit the Getting the answers you need section of our provider microsite.
Visit the Sleep provider microsite to access helpful information and tools such as a direct link to the provider portal, clinical guidelines, FAQs and more.
PAP Device Replacements Reminder
To help ensure your practice has correct and current information on our Sleep Program, our Carelon Sleep leads want to provide a reminder on our review requirements for Positive Airway Pressure (PAP) device replacements.
While Carelon does review for initial treatment requests for PAP devices, we do not review for replacement devices. Please check with your health plan representative to determine if they have review requirements for replacement devices. You can also have your patients contact their Member Benefits number on the back of their ID card to determine the coverage for device replacement.
Carelon’s Sleep and Additional Outpatient UM Programs have been upgraded to our new and improved platform
We’re pleased to share that on November 1st, our Sleep and Additional Outpatient Programs were migrated to a new and improved platform for submittal and review of requests.
Our new platform and system engine were designed to deliver an improved and more efficient provider experience for you. We’ve introduced an expanded procedure code selection and enhanced intake screens with specific questions to guide providers and other portal users through the correct service selection and clinical scenarios.
Portal enhancements
Prior to the migration, the button to access Sleep and Additional Outpatient UM letters was located below our View Order Summary button:
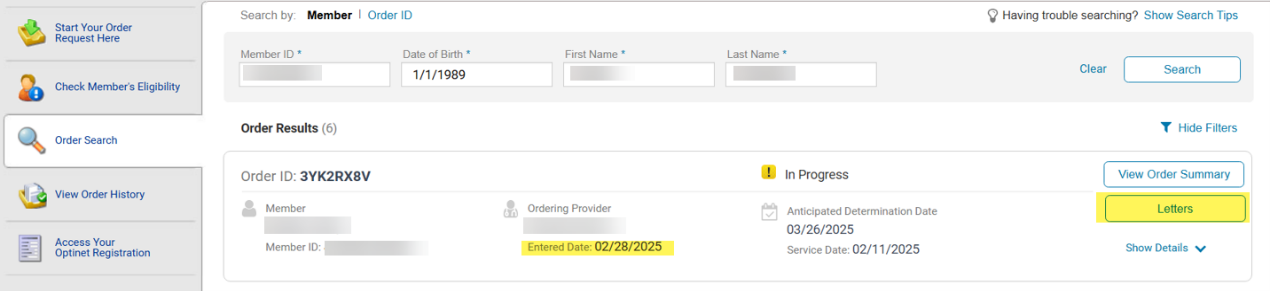
With the migration complete, the letters button has been removed from the former location and moved to a more convenient section that matches the location of our other solutions.
For Sleep and Additional Outpatient UM cases created on or after March 1, 2025, portal users will now click on the View Order Summary button to access and view letters:
Important Reminder:
As we close out our platform migration, please remember to clear your cache if you experience any system task issues. These can occur and are temporary. Once the cache is clear, please try the task again, which resolves the issue.
New Sleep codes available 11/1/25:
If you received notice of new sleep codes being introduced Q4, please note that they will be available for requests in our system 11/1/25 for health plans who have adopted them.
Upcoming training opportunities
Providers are invited to see a demo of the new platform at our upcoming training sessions.
Sign up today on the Resources page of our Sleep provider microsite or via the Provider Connections Training page.
Be sure to check the provider microsite for additional information including updated program FAQs coming soon.
Sleep durable medical equipment (DME) – How we manage PAP compliance
Carelon Medical Benefits Management (Carelon) is continually looking for ways to enhance the provider experience by ensuring an efficient order request entry and adjudication process.
With that in mind, Carelon’s sleep solution offers management of obstructive sleep apnea from diagnosis to treatment options. If the best treatment is determined to be the use of a positive airway pressure machine (PAP), then Carelon monitors member compliance of device usage through an automated process that saves durable medical equipment (DME) providers time when requesting future authorizations.
As a reminder, the DME provider needs to select Carelon Medical Benefits Management (AIM Specialty Health) on the manufacturer’s site to match the member to Carelon. This could be listed as different fields on each manufacturer’s site. For Phillips devices, Carelon is listed under ‘external services’ on the manufacturer’s site and for ResMed, Carelon (AIM Specialty Health) is listed under ‘add integrator details.’
When a member is diagnosed with obstructive sleep apnea and requires treatment with a PAP (positive airway pressure) device, the request is reviewed for medical necessity by Carelon. The request is authorized if it meets medical necessity review. The DME provider then registers the device to the member within the manufacturer’s website, using member demographic data and instructs the manufacturer site to match the member data to Carelon (AIM Specialty Health), which validates the member data within Carelon’s system.
This allows Carelon’s system to receive member and manufacturer data from the manufacturer’s site. Carelon then utilizes this information when a subsequent request is entered for ongoing PAP supplies and pre-populates member device usage data within the request, which saves providers time and makes entry of the order request more efficient.
For more information on the sleep program, including how to enter an order request, please visit the provider microsite.
Reminder: Sleep program equipment recall notice still in effect – March 2023
On June 14, 2021, Philips Respironics issued a voluntary recall on specific brands of their CPAP/APAP, BiPAP machines. Philips has established a registration process that allows patients, users, or caregivers to look up their device’s serial number and initiate a claim if their unit is affected.
To view the recall information and register your device, use the following link: https://www.usa.philips.com/healthcare/e/sleep/communications/src-update
We will keep you informed of future updates related to this recall on our provider microsite.
Visit the Surgical Procedures provider microsite to access helpful information and tools such as a direct link to the provider portal, clinical guidelines, FAQs and more.
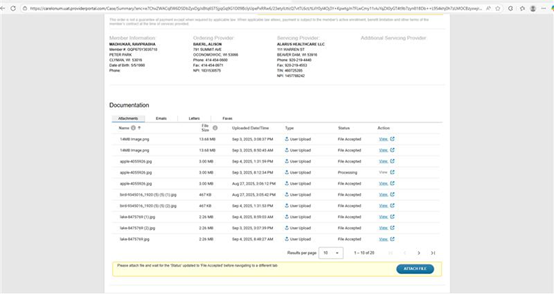
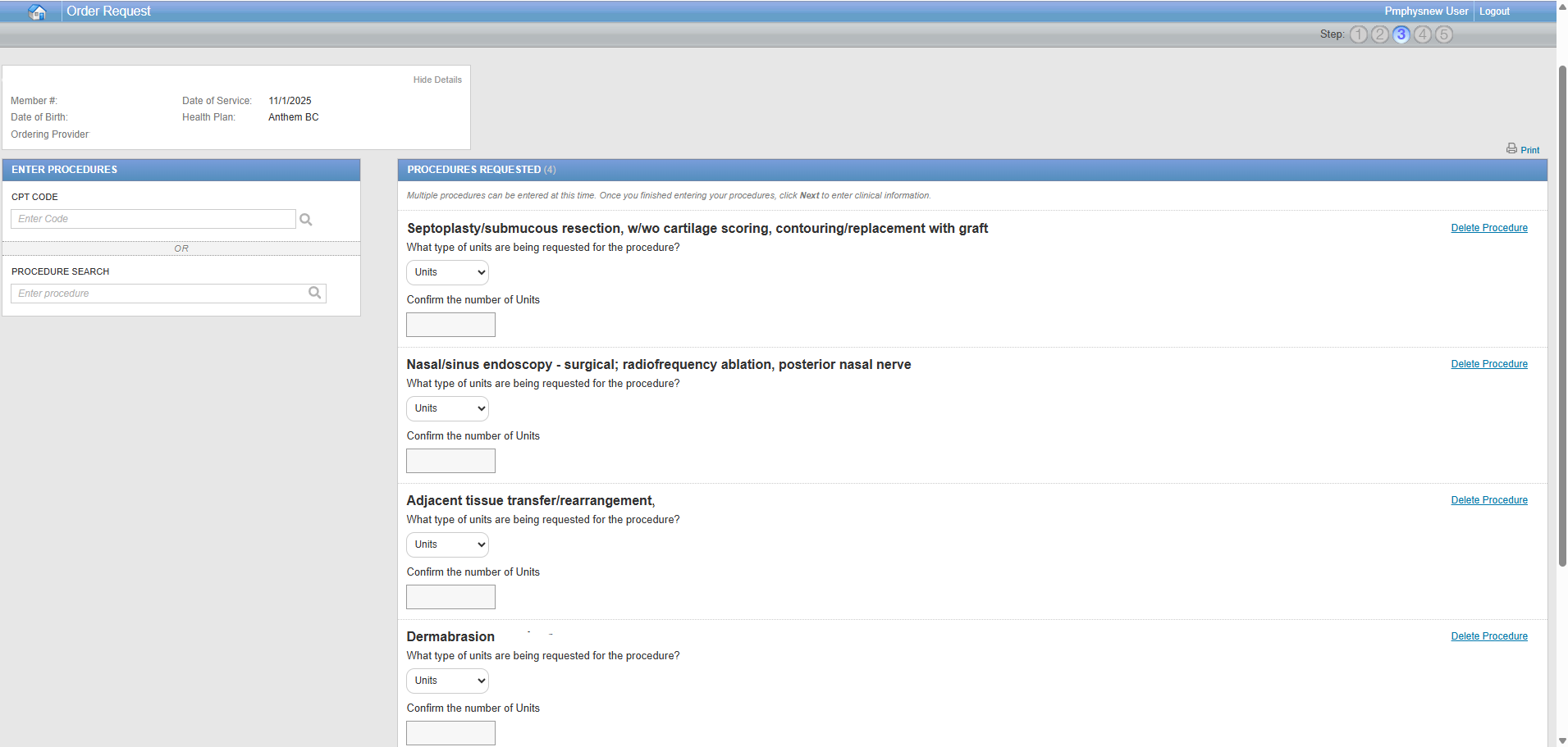
You asked for it, we delivered: Surgical Program enhancement implemented – You can now enter the number of units per CPT code
Effective today, our system will allow you to specify the quantity of units per CPT code for certain surgical procedures. This enhancement includes procedures in specialties such as Ear, Nose, and Throat, as well as Plastic and Reconstructive Surgery, among others. Please note that these new fields will apply across a wide range of procedure codes.
By specifying the units, you can ensure greater accuracy in alignment between authorizations and claims. Units entered will be saved to each case and can be easily downloaded or printed on the Order Summary. This improvement is part of our ongoing commitment to providing you with an organized and efficient platform.
- Our main purpose is to deliver an organized way to align information between authorizations and claims. Payment is still subject to the health plan’s reimbursement policies and the member’s active enrollment.
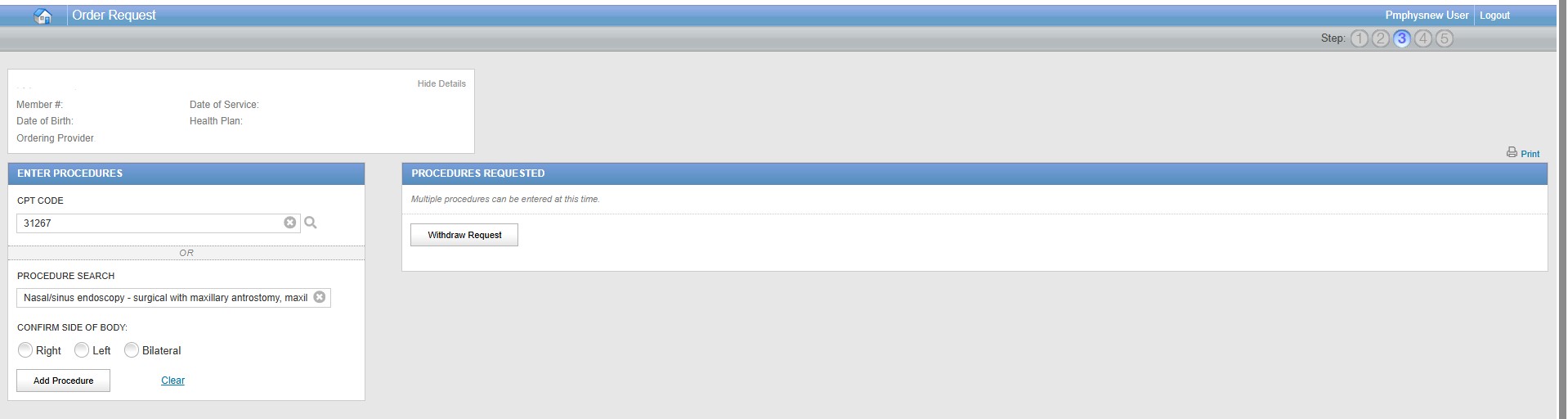
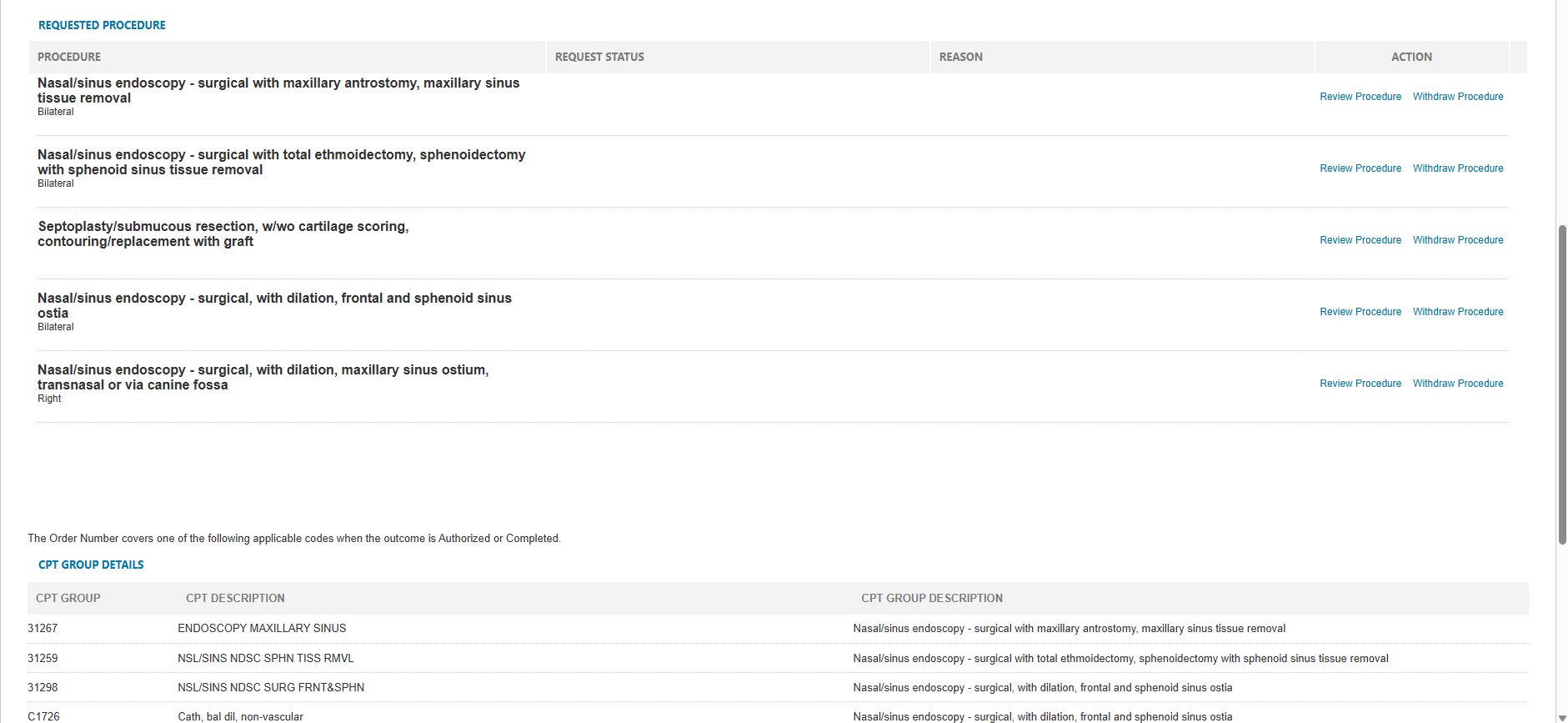
Reminder: Surgical procedure update – Confirmation of Side of Body/ Laterality
As a reminder, this past June, we implemented an update to our Surgical program: Certain Surgical procedures now include a requirement to confirm the side of the body and laterality (left, right, or bilateral).
Key updates implemented:
- The portal now allows or prevents duplicate CPT code selection, based on the side of the body selection.
- CPT code modifiers are now automatically applied to reflect the appropriate side of the procedure.
Examples:
Tips for maintaining a smooth provider portal experience:
- Reboot daily – most programs have releases where new or existing functionality is updated; rebooting ensures that those most recent updates are reflected in your computer.
- Clear cookies and cache – periodically clearing your cookies and cache can keep your computer “clean” and promote efficiency. If you don’t know how, contact your IT department.
- Use the right browser – Use Google Chrome for optimal use of the provider portal. Please note that Internet Explorer (IE) has been retired.
Peer-to-peer requests / Specialty-matched provider consultations:
Requests that do not meet medical necessity criteria: When an order request cannot be approved immediately, you will have the option of discussing your case with one of our clinical experts. A peer-to-peer discussion with one of our Carelon clinician reviewers is always offered before any adverse determination is made. No adverse determination is made until the case has been reviewed by a clinician reviewer at Carelon.
It is important that when the Carelon clinician reviewer informs your office (always via phone or fax), that the case pends for peer-to-peer conversation, your ordering physician calls Carelon as soon as possible to discuss it with a Carelon clinician reviewer. Until we receive a phone call back, the case will continue to pend until it is due to close in accordance with health plan requirements. Urgent requests will pend for up to 72 hours after initial receipt of the case. At the time of required case closure, if the clinical information requested is not provided and/or peer-to-peer did not take place, the case will be denied. Denial letter will be sent to the member and provider.
How will we know when a peer-to-peer is needed?
When a case pends for review, it will go to an “In Progress” status. Carelon will request the ordering provider requesting a call-back for peer-to-peer review, should it be required.
More Information – Where can I access additional information?
For assistance contact us by email or at 800-252-2021.