All Solution Tips and Tricks
All of our provider microsite links are posted on the Carelon provider portal, but did you know that our Provider Connections news blog is accessible from each solution’s microsite? Microsites are mini websites that give information about Carelon solutions, such as Radiation Oncology. You can access the News blog site to see our current and past issues of Provider Connections.

Evidence assessment:
Did you know that the Carelon MBM Guideline Development team conducts a systematic evidence review to inform both new guidelines and annual updates? A key component of the process is an assessment of the collected evidence by a trained methodologist using standardized tools such as Quality Assessment of Diagnostic Accuracy Studies (QUADAS), Standards for Reporting of Diagnostic Accuracy (STARD), Diagnostic Accuracy Quality Scale (DAQS), and the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE).
These tools provide a systematic way to determine whether a particular article meets the standard of quality needed to inform clinical decision-making. They take into account such factors as bias, the size and composition of the study group, and the statistical methods used to evaluate the findings.
For more information on our evidentiary review process, visit our Clinical Guidelines and Pathways page, clinical guidelines access section: https://guidelines.carelonmedicalbenefitsmanagement.com/
Did you know?
Available 24/7, each of our MBM solution microsites include valuable resources for you and your peers.
Visit our Resource pages to learn more about our programs and access helpful information and tools including:
- Order entry checklists
- Clinical guidelines
- Direct access to our MBM provider portal and clinical guidelines
- FAQs and more
Updates are applied to our solution microsites frequently, so we encourage you to visit them often to ensure you have the latest program information available.
For easy future reference, be sure to bookmark the Resources page/s that match your specialty.
MBM solution provider microsite Resources links:
- Radiology provider website: https://providers.carelonmedicalbenefitsmanagement.com/radiology/
- Cardiovascular provider website: https://providers.carelonmedicalbenefitsmanagement.com/cardiovascular/
- Sleep provider website: https://providers.carelonmedicalbenefitsmanagement.com/sleep/
- Musculoskeletal provider website: https://providers.carelonmedicalbenefitsmanagement.com/musculoskeletal/
- Rehabilitation provider website: https://providers.carelonmedicalbenefitsmanagement.com/rehabilitation/
- Genetic Testing provider website: https://providers.carelonmedicalbenefitsmanagement.com/genetictesting/
- Radiation Oncology provider website: https://providers.carelonmedicalbenefitsmanagement.com/radoncology/
- Medical Oncology provider website: https://providers.carelonmedicalbenefitsmanagement.com/medicaloncology/
- Surgical provider website:
https://providers.carelonmedicalbenefitsmanagement.com/surgicalprocedures/
Have you visited our Carelon Medical Benefits Management website recently? Check out the latest updates for providers.
Another great complimentary resource you may want to bookmark is our Carelon Medical Benefits Management website for continued easy access to our provider portal and tools, new program information, important program enhancements, training opportunity news, access to our Provider Connections news blog and more: https://www.careloninsights.com/medical-benefits-management/specialty-care
There is a convenient Providers drop down menu in the navigation bar that provides quick access to such tools as:
- Carelon MBM clinical appropriateness guidelines and pathways*
- Our provider resources access page
- Carelon MBM provider portal
*From our clinical appropriateness guidelines and cancer treatment pathways page, you can now conveniently toggle between our Provider Connections blog page and the guidelines page.

Direct access to Carelon Post Acute Solutions program info and provider resources
Through our post acute care programs, we ensure patients receive quality, seamless care when and where they need it most, such as the home or a post-acute care facility..
We do this by working with providers like you or our own local network to align care with the latest evidence and health plan care management plans.
If you service post-acute solutions members, you’ll also find convenient access from our Providers drop down menu to:
Solution-specific tips you can use
Visit the Back Pain Program provider microsite to access helpful information and tools such as a direct link to the provider portal, clinical guidelines, FAQs and more.
Reminder: Imaging & Management of Low Back Pain provider video now available within MBM provider portal*
Do you ever question the need for imaging when a patient complains of low back pain, or wonder what imaging or treatments to start with? In this short 15-minute video on Imaging & Management of Low Back Pain, we discuss the etiologies of low back pain, clarify the role of imaging and associated harms/risks, and review current evidence-based treatment recommendations.
To access this video, please go to the Provider Portal® home page and login then navigate to the Help Center > Provider Webinars > All Solutions section. Finally, click on “Imaging & Management of Low Back Pain Training” to watch the video. Once you have completed the video, please complete this survey link to help us determine if the video was helpful. Your feedback* helps our content development in the future.
You can also access the training video on our blog page here.
*Survey feedback and participation may be shared with your health plan.
Visit the Cardiovascular provider microsite to access helpful information and tools such as a direct link to the provider portal, clinical guidelines, FAQs and more.
Reminder: Our Cardiology Solution will be renamed to Cardiovascular Solution effective this July
If you work with our Cardiology Solution, please note that over the next two months you will notice a name change being applied wherever referenced. The new name, Cardiovascular Solution, is being applied in our MBM provider portal, training materials, and other documentation. Our provider microsite name and URL have also been updated to include the new Cardiovascular name: https://providers.carelonmedicalbenefitsmanagement.com/cardiovascular/.
Our health plan clients often use customized names for their programs with us. They’re permitted to select the best program name that works for them, so you may continue to see some usage of Cardiology Program on health plan websites.
Reminder notices will remain programmed on our Provider Connections blog and on our Cardiology provider microsite through close out of the name transition.
Visit the Genetic Testing provider microsite to access helpful information and tools such as a direct link to the provider portal, clinical guidelines, FAQs and more.
Harvard Pilgrim providers: Please visit the Harvard Pilgrim Genetic Testing provider microsite.
Reminder: Genetic Testing Program updates coming soon
Effective August 1, 2025, the following update will apply to the Carelon MBM Genetic Testing Program. The service date (i.e., DOS) will be defined as the sample or collection date across all lines of business. For archival samples, the sample collection or retrieval date will serve as the DOS for review. In the rare circumstance that an exception is needed, providers may reach out to the Carelon MBM genetic testing team at DL-GeneticTestingSolution@carelon.com.
This update is focused on providing clinically appropriate, safe, and affordable health care services. Providers are reminded that they may submit authorization requests through the Carelon provider portal at www.providerportal.com. Portal access is available 24/7 to process requests in real-time and is the fastest, most convenient way to request an authorization.
Genetic Testing OptiNet application will be retired late July
As of Saturday, July 27th, the Carelon Genetic Testing (GT) OptiNet application tool will be retired and will no longer be available for the use of registering genetic counselors. GT OptiNet users will no longer be able to access their registrations as the GT OptiNet application will be removed.
Please note: This change will not have any impact on Genetic Testing prior authorizations via the Carelon provider portal online tool or the Carelon call center.
If you have any questions, please do not hesitate to contact our OptiNet assessment team at: 877.202.6543 or email us at Assessment@carelon.com
July 2024 changes to the Anthem/Amerigroup/Wellpoint Genetic Testing Program
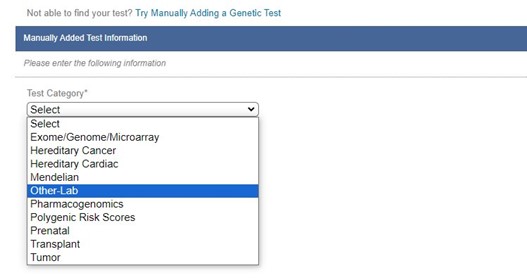
Addition of new test category/sub-category
To support the review of non-genetic laboratory testing for Anthem/Amerigroup/Wellpoint plans, Carelon has recently added a new test category and subcategory of Other-Lab/Other-Lab when manually adding tests. These should ONLY be selected when submitting requests for the following CPT codes when requesting services that are covered by the Anthem medical policies Topographic Genotyping and Metagenomic Sequencing for Infectious Disease in Outpatient Settings. The following CPT codes will be reviewed under these policies: 81479, 81599, 84999, 87999, 0112U, 0152U, and 0323U.
Retirement of genetic counseling functionality
To better align with the Carelon Genetic Testing clinical guidelines, we are currently only asking an attestation about counseling during the clinical question portion of the process when appropriate. Information on date of counseling and counselor name/organization will no longer be required.
Change in sample collection date/date of service collection*
*Please note: This change has been delayed. We will provide updates once available.
The Carelon MBM Genetic Testing Program will be changing our definition of service date (i.e., DOS) to sample or collection date to align with the CMS Laboratory date of service policy, which specifies that the DOS is the date the specimen was collected. For archival samples, the sample collection or retrieval date will serve as the DOS for review. Our operations team will immediately be manually making this update with changes to our portal to follow shortly. If an exception is needed, please contact Carelon Medical Benefits Management at DL-GeneticTestingSolution@carelon.com.
On July 29, 2024, we will update the service date directions in the portal for genetic testing as follows:
Current: For genetic testing, use the testing date.
New: For genetic testing, use the sample collection or retrieval date in alignment with the CMS Laboratory date of service policy. For an exception, please contact Carelon Medical Benefits Management.
CMS policy 40.8 Date of Service 9DOS) for Clinical laboratory and Pathology Specimens
(Rev. 4881; Issued 12-20-19, Effective 01-01-20, Implementation: 01-23-20)
Assistance with manually adding a genetic test
At the beginning of the year, we made changes to how users were able to manually add genetic tests for review. Users are now required to select a “test category” and “test sub-category” when adding a test. This is to help ensure we are reviewing the request appropriately.
However, some users have had issues correctly selecting the test category and sub-category. Your best resource for choosing these correctly would be to discuss with the ordering physician or a genetic counselor. If these resources are unavailable to you, we have put together a Test Category tip sheet, which is now available for use in the provider portal.
After Clicking on “Try manually adding a test,” you will now see the link below to “view test category and sub-category detail.” The link will open in a new window or browser tab.
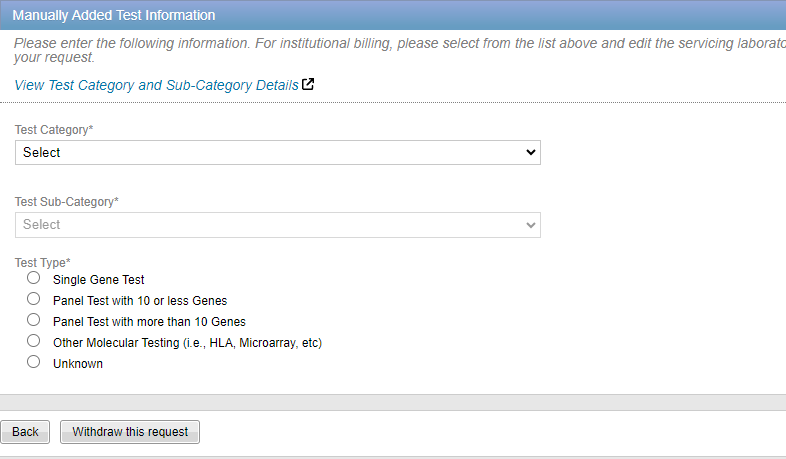
Many commonly ordered types of tests are listed to assist you with selecting the correct details. Key words are listed for each test type. This list will be updated regularly throughout the year, so please click the link each time you need to manually add a test.
Introducing our new Genetic Testing Program clinical engine
The Carelon Genetic Testing Program is proud to announce the launch of our new clinical engine. The development of this new clinical engine allows us the ability to not only deliver a number of key enhancements making the process more accurate and efficient, but also provides us an opportunity to better categorize data, offer more configurability, and provide the structure for more agility for future enhancements.
Along with the development of this new clinical engine, we have also expanded our team to include nearly fifty board-certified genetic counselors, making Carelon MBM one of the top centers of expertise in genetics throughout the nation.
This expansion allows not only a level of genetic testing review expertise unmatched in the market today, but also the best possible provider-centric service for our ordering physicians to discuss their questions surrounding genetic testing.
To learn more about the genetic testing program, please visit our provider site at https://providers.carelonmedicalbenefitsmanagement.com/geneticsandlaboratory/.
Our provider microsites provide access to helpful information and tools such as a direct link to the provider portal, clinical guidelines, FAQs and more. Contact your health plan representative for the program link applicable for their Carelon Medical Oncology program.
Carelon Medical Oncology Program drug entry – regimen abbreviation list now available on provider microsite
For your convenience, our Medical Oncology team has prepared a new Regimen Abbreviation document that can assist with the drug entry on process on the Requested Services screen.
You can find it under our Resources page here.

Additional Medical Oncology Program documents we have posted for easy reference for you and your practice include:
-
- Program overview
- Quick guide to order entry
- How to register for provider portal
- Steps to get your practice ready checklist
- How to submit a pathway inquiry
Be sure to bookmark our Medical Oncology provider microsite Resources page for future reference.
Archived articles
View past Medical Oncology Tips articles here.
Visit the Musculoskeletal provider microsite to access helpful information and tools such as a direct link to the provider portal, clinical guidelines, FAQs and more.
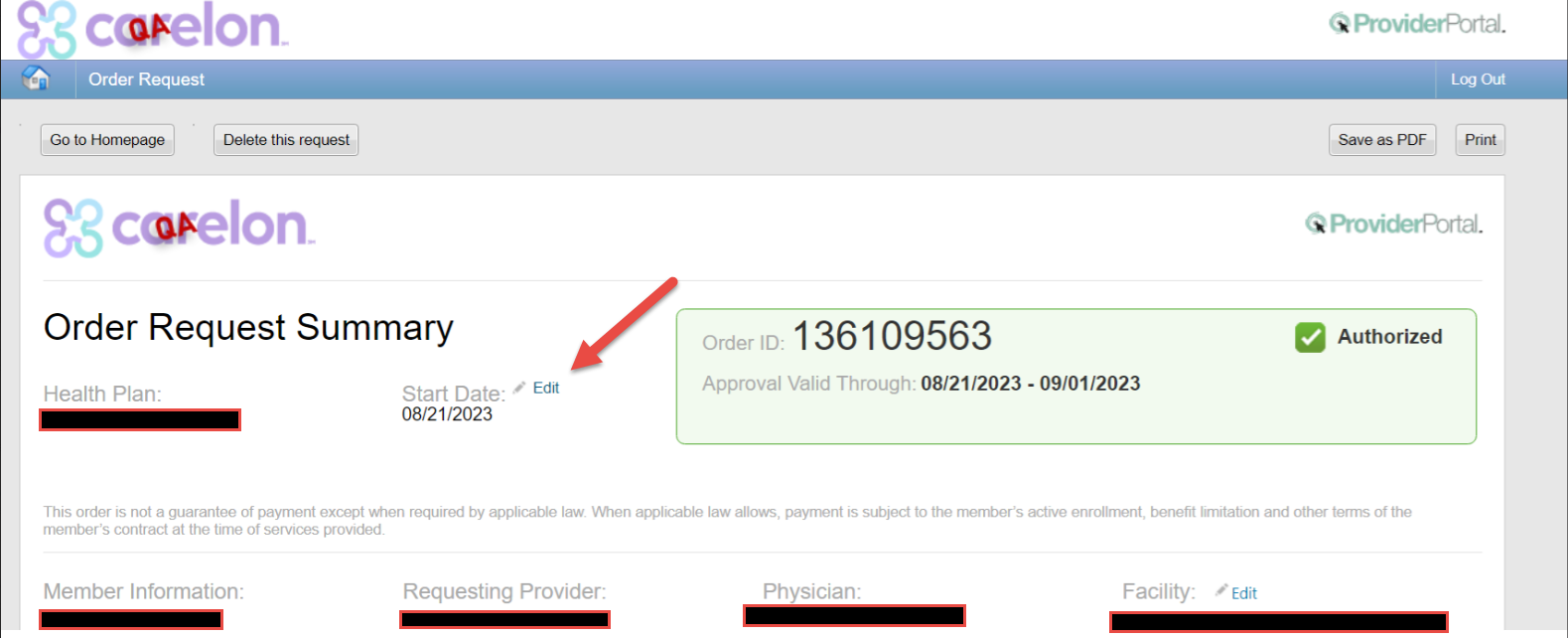
What’s new in the Musculoskeletal Program?
Our dedicated Musculoskeletal Program team has prepared some helpful tips and updates for you and your team members.
New enhanced functionality:
Our Musculoskeletal Program now allows the date of service to be changed on our provider portal for approved prior authorizations. We recognize that surgical dates can change and wanted to make it easier for providers to make this update without having to call Carelon.
Tip #1: The top five critical ingredients we need you to send to help authorize your case are:
-
- Your physician’s note needs to describe the exact surgery being planned, and the reason the surgery is needed.
- The note needs to say when the patient started having pain/symptoms, the severity of the pain, and how the pain effects the patient’s activities.
- The note needs to include an assessment of the physician’s recent exam of the painful area.
- The note needs to tell us what type of treatment the physician prescribed, how long the patient tried the treatment, and if the treatment improved the patient’s pain/symptoms.
- A copy should be sent of the radiologist’s report of any recent x-ray, CT, MRI, or ultrasound ordered by the physician to diagnose the reason for the pain/symptoms.
If any of these are missing, we may not have enough information to authorize your case.
Note: For a procedure to be pre-authorized, the notes have to show that your patient has the symptoms, exam, treatment, and imaging that meet Carelon’s criteria for the surgical procedure you are requesting. You can view the criteria at: (put in link for Joint guidelines).
Tip #2: Did you know that some procedures must have a radiologist report for pre-authorization?
If your doctor ordered a CT scan or MRI to find out the reason your patient has pain/symptoms, you need to send us a copy of the radiologist’s report.
Some offices copy and paste the report’s “impression” into their Electronic Medical Record (EMR). The impression does not always include important information that is in the rest of the report.
To avoid delays with your authorization request, remember to submit the radiologist’s report.
Providers can check the microsite for 2023/2024 quarterly session dates and sign-up for a future training session on our Musculoskeletal Program microsite.
Visit the post-acute provider microsite to access helpful information and tools such as a direct link to the provider portal, provider materials, program information and more.
PAC-IM program survey opportunity: We want to hear from you!
Carelon is pleased to offer a survey opportunity for current PAC-IM program participants. Be sure to share your skilled nursing facility’s strengths and capabilities to help us improve patient care.
Anthem providers: Please access the survey here – Take the survey now!
BCBSRI providers: Please access the survey here – Take the survey now!
Cambia providers: Please access the survey here – Take the survey now!
Wellpoint providers: Please access the survey here – Take the survey now!
The survey is quick and convenient, and can also be accessed from our post-acute programs provider site. Thanks for your participation!
Social Drivers of Health (SDoH) Program update
Carelon is excited to share the release of our updated Social Drivers of Health (SDoH) Assessment and updated self-paced provider training. The enhancements are designed to improve your experience and the quality time spent with our members.
Key changes Include:
- Streamlined approach: The updated format simplifies the process, making it more intuitive and user-friendly.
- Consolidated questions: We have refined our question set to reduce redundancy, ensuring that your interactions with members are more meaningful and focused.
- Improved assessment process: By consolidating and optimizing questions, we’ve decreased the time required to complete assessments, allowing for deeper and more impactful engagement with members.
We are confident these improvements will not only facilitate more effective care management but will also enhance your ability to connect with members in a more meaningful way.
Please feel free to reach out to HHprovider_relations@carelon.com if you have any questions or require further information regarding these updates.
Archived articles
You can view recent post-acute provider updates here:
Visit the Radiation Oncology provider microsite to access helpful information and tools such as a direct link to the provider portal, clinical guidelines, FAQs and more.
Archived articles
View past Radiation Oncology Tips articles here.
Visit the Radiology provider microsite to access helpful information and tools such as a direct link to the provider portal, clinical guidelines, FAQs and more.
Now live: OptiNet December release enhancements implemented
As you know, OptiNet helps with site servicing selection!
When we at Carelon MBM are contacted to order imaging studies, we offer the information we collect in OptiNet to help locate clinically appropriate, convenient, and cost-effective alternate imaging study facilities for patients, so please be sure to always keep your registration complete and current.
Why are we reaching out?
For our provider portal users who are also registered in OptiNet, we want to inform you about some enhancements / changes we’ve made to the application.
What changed?
- Effective December 16, 2023, OptiNet will no longer auto display providers, but will require a search. This will minimize the number of records displayed.
- OptiNet providers will now have the option to search by site location or registration ID.
What does this mean?
- OptiNet providers will have the ability to search by specific registration numbers! When being notified about registrations requiring an update, this search will take you directly to your site.
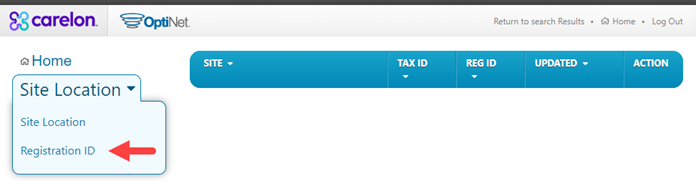
- Rebranding of some health plans will take place with the start of the new year. Therefore, you may notice your health plan name displaying differently within the OptiNet dropdown.
What’s next?
- Be on the lookout for further enhancements within OptiNet.
- Check out our helpful Guide section for additional OptiNet documentation.
- Any changes we make within our OptiNet application is to make it more user-friendly! We hope these changes help you navigate within the application easier.
If you have any questions, please do not hesitate to contact our OptiNet assessment team at: (877) 202-6543 or at Assessment@carelon.com.
Don’t wait. Register your imaging site of care with OptiNet today!
Carelon understands the key role that medical practices play in the delivery of care for patients who require imaging studies. Developed in collaboration with health plans, our Radiology Program helps support quality care that is consistent with current medical evidence and delivered in the most clinically appropriate setting.
Our program includes OptiNet, which is available in the provider portal. OptiNet is a proprietary, multifaceted program designed to collect service and capability information on outpatient imaging providers.
About OptiNet
Available to our health plan clients, OptiNet is the Carelon assessment tool that gives providers more transparency when ordering high-tech imaging procedures and more. OptiNet generates a modality score based on equipment, staffing, and quality control information reported by the facility.
It is available in the provider portal.
Register your imaging facility today!
Choosing an imaging provider is an important decision for our customers, affecting the quality and cost of their care. The Carelon OptiNet tool will help providers and their patients compare high value, lower cost imaging facilities for computed tomography (CT) imaging, magnetic resonance (MRI) imaging, and other imaging services.
Why is registration important?
When you register, your facility information is displayed in the provider portal. By registering, your facility may be available on our Initial Display List to ordering physicians and members requesting imaging services. Providers register sites within OptiNet to become eligible alternate sites for our Site of Care and Carelon Specialty Care Shopper (member engagement) programs.
What do you need to do?
Register in the OptiNet tool.
How to register
- Log in to the provider portal at https://providerportal.com.
- Select “Access Your OptiNet Registration” found on the left-hand side of the provider portal home page.
- OptiNet will guide you through the registration process.
What data will be included?
The Carelon online registration tool, OptiNet collects data on imaging providers related to facility specifications, technologist and physician qualifications, accreditation, equipment features, and technical registration. This information is used to determine how organizations conform to industry-recognized standards, including those established by the American College of Radiology (ACR) and the Intersocietal Accreditation Commission (IAC).
For more Information:
View our provider microsite to learn about the many benefits of OptiNet.
If you have any questions about the OptiNet registration or score card generation, please contact the Carelon Assessment Department at 877.202.6543 or by email at Assessment@aimspecialtyhealth.com.
OptiNet brand update
Last year, we introduced our new company name, Carelon Medical Benefits Management (MBM). Carelon is our multi-faceted healthcare services brand dedicated to solving the industry’s most complex challenges.
As a follow up to this rebranding, you may soon notice that our former OptiNet branding is now being shown as OptiNet. This is a name appearance change only and does not impact any functional changes to the program.
OptiNet is our online assessment tool designed to collect service and capability information. It is a self-reporting tool for servicing providers to report information offered at their imaging and genetic testing locations and to assist with ordering providers search results during site selection for pre-authorization orders. The information collected helps to support the Carelon MBM site of care program, Specialty Care Shopper OptiNet initial display, and imaging credentialing programs.
Visit the Rehabilitation provider microsite to access helpful information and tools such as a direct link to the provider portal, clinical guidelines, FAQs and more.
Rehabilitation program tips
Rehabilitation providers: For easy reference, here is a summary of recent information added to our FAQs posted on the rehabilitation microsite.
Rehabilitation program updates: What’s new at Carelon Medical Benefits Management?
We have implemented some enhancements to our Carelon MBM Rehabilitation program that we’re excited to share with you!
We recently updated the Rehabilitation provider search functionality within therapy requests. Previously, users were asked to name the billing entity, and if applicable, were also asked to enter the treating therapist for the request. Following the update, users are only being asked to enter the provider who is selected as the billing entity for the request.
The Rehabilitation program recently completed a clean-up of therapy requests that had been initiated by a portal user, but not submitted. Carelon canceled out any incomplete requests that were open for more than seven days.
If the user pulls up one of the canceled requests, they will get a message letting them know it was canceled due to being open for more than seven days, “This request was canceled due to being open more than seven days. If the service is still needed, please start a new request.” If skilled services are still required, the user will need to submit a new request.
How often should providers update the episode of care initial evaluation date in the Carelon portal for members receiving long-term therapy services?
Within the Carelon rehabilitation program, requests are staged based on the initial evaluation date of service as well as the previous request for medical necessity determination. For these reasons, providers are asked to keep the initial evaluation date consistent throughout the member’s episode of care when submitting prior authorization requests for additional treatment.
There is one scenario in which the initial evaluation date may change and that is typically for chronic, long term or pediatric episodes of care that extend past a calendar year of treatment. In these scenarios, there is a reasonable expectation that the initial evaluation and plan of care would be updated annually. The updated initial evaluation date should also be documented annually within in the member’s therapy treatment requests on the Carelon portal.
What should a provider do if they have not received the request determination, but the patient is scheduled to return for treatment soon?
If a provider has not received a determination on their request and the patient is returning to the facility, the provider may contact the Carelon Call Center and ask that the request be reviewed live. If the provider is unable to hold while the request is reviewed, the provider facility can request a call back once the review is completed.
What are the most common reasons a second treatment prior authorization request receives a lower visit allocation (i.e., 2-4 visits)?
When a second treatment request received a lower than typical visit allocation, there are a few possible reasons for this outcome.
-
-
- Did the provider document an in-scope functional outcome tool (from the microsite list) on the initial treatment request and document a baseline score?
- Did the provider reference the scoring scale on the provider microsite to ensure that the functional outcome tool score documented matched the scoring scale that Carelon utilizes?
- Did the provider document an in-scope functional outcome tool (from the microsite list) on the second treatment request and document an updated score from the member’s most recent visit?
- Did the provider document a mitigating factor in the event of little to no progression documented on the functional outcome tool score between the initial or second treatment requests?
- Did the provider document a change to the plan of care in the event of little to no progression documented on the functional outcome tool score between the initial or second treatment requests?
- Did the provider document short-term goal achievement on the second treatment request?
- Has a benefit limit been reached, where benefit limits apply?
- Has the member achieved the plan of care functional goals when two visits may be appropriate for discharge planning and home exercise program instruction?
-
The provider has the option to call Carelon at any time for a peer-to-peer discussion if they feel the details of their request need to be clarified.
To access our full set of rehabilitation program FAQs, visit the Getting the answers you need section of our provider microsite.
Visit the Sleep provider microsite to access helpful information and tools such as a direct link to the provider portal, clinical guidelines, FAQs and more.
Coming soon: Carelon’s Sleep Program will be upgraded to our new and improved platform Q3 2025
Effective this fall, sleep program providers will experience a new and improved platform for submittal and review of sleep program requests.
Transition to our new platform will enhance the provider experience during intake process through provider portal. There will be an improved procedure code selection and enhanced intake screens with specific questions to guide providers and other portal users through the correct service selection and clinical scenarios.
Upcoming training opportunities
Providers are invited to see a preview of the new platform at our upcoming training sessions, which are being offered this July and August.
Each training session will include an overview of the updates and intake process. Sign up today on the Resources page of our Sleep provider microsite or via the Provider Connections Training page.
Training dates:
Be sure to check the provider microsite for additional information including updated program FAQs coming soon.
Sleep durable medical equipment (DME) – How we manage PAP compliance
Carelon Medical Benefits Management (Carelon) is continually looking for ways to enhance the provider experience by ensuring an efficient order request entry and adjudication process.
With that in mind, Carelon’s sleep solution offers management of obstructive sleep apnea from diagnosis to treatment options. If the best treatment is determined to be the use of a positive airway pressure machine (PAP), then Carelon monitors member compliance of device usage through an automated process that saves durable medical equipment (DME) providers time when requesting future authorizations.
As a reminder, the DME provider needs to select Carelon Medical Benefits Management (AIM Specialty Health) on the manufacturer’s site to match the member to Carelon. This could be listed as different fields on each manufacturer’s site. For Phillips devices, Carelon is listed under ‘external services’ on the manufacturer’s site and for ResMed, Carelon (AIM Specialty Health) is listed under ‘add integrator details.’
When a member is diagnosed with obstructive sleep apnea and requires treatment with a PAP (positive airway pressure) device, the request is reviewed for medical necessity by Carelon. The request is authorized if it meets medical necessity review. The DME provider then registers the device to the member within the manufacturer’s website, using member demographic data and instructs the manufacturer site to match the member data to Carelon (AIM Specialty Health), which validates the member data within Carelon’s system.
This allows Carelon’s system to receive member and manufacturer data from the manufacturer’s site. Carelon then utilizes this information when a subsequent request is entered for ongoing PAP supplies and pre-populates member device usage data within the request, which saves providers time and makes entry of the order request more efficient.
For more information on the sleep program, including how to enter an order request, please visit the provider microsite.
Reminder: Sleep program equipment recall notice still in effect – March 2023
On June 14, 2021, Philips Respironics issued a voluntary recall on specific brands of their CPAP/APAP, BiPAP machines. Philips has established a registration process that allows patients, users, or caregivers to look up their device’s serial number and initiate a claim if their unit is affected.
To view the recall information and register your device, use the following link: https://www.usa.philips.com/healthcare/e/sleep/communications/src-update
We will keep you informed of future updates related to this recall on our provider microsite.
Visit the Surgical Procedures provider microsite to access helpful information and tools such as a direct link to the provider portal, clinical guidelines, FAQs and more.
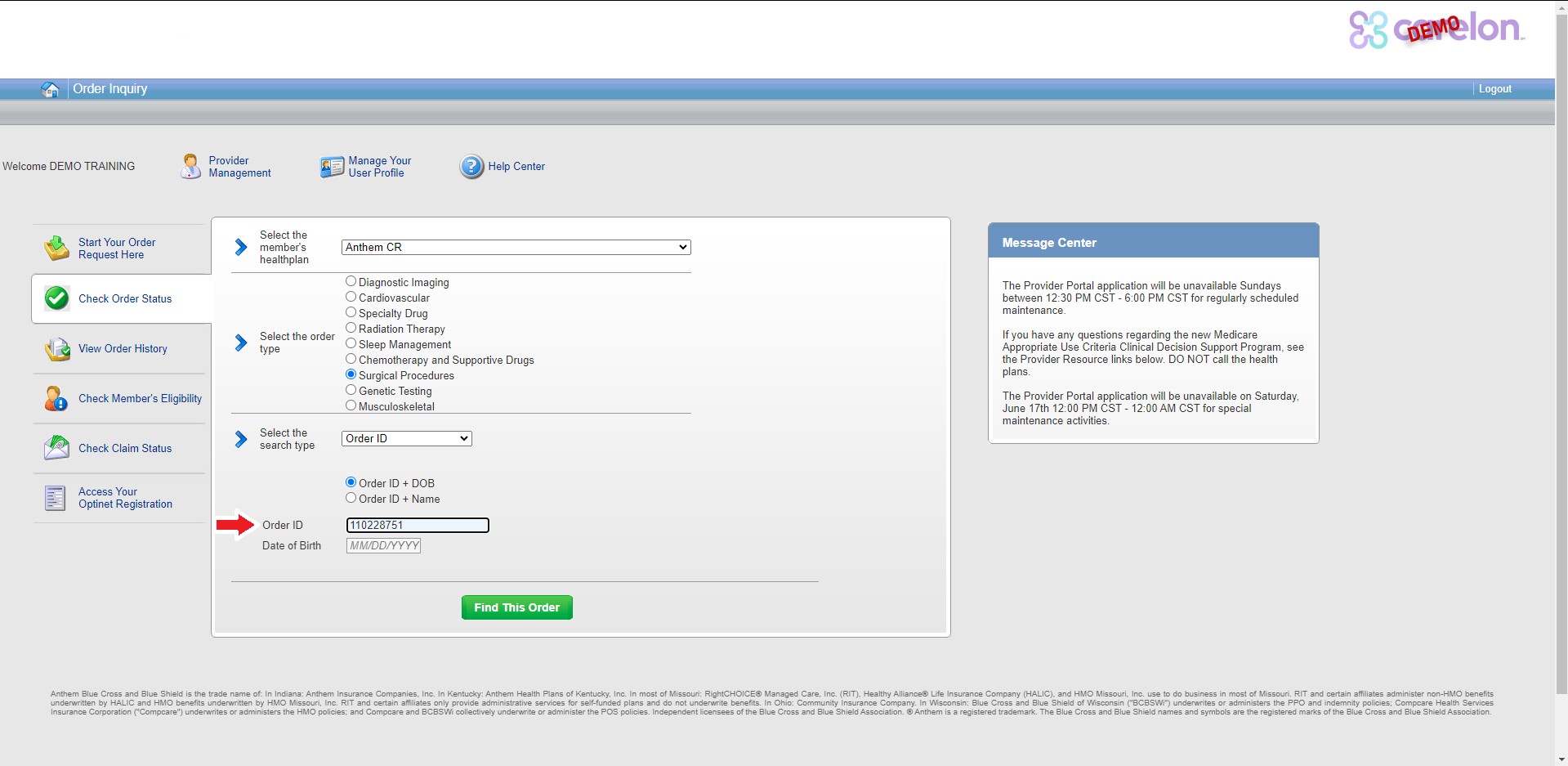
Upcoming change to order ID’s – surgical program
We’ve made a recent change to our surgical program. Order ID’s for Carelon’s surgical program are distinguishable by the letters “SU” preceding a 9-digit number. However, the numerical portion is all that’s necessary to find an order.
Beginning July 15, 2023, you only need to enter the 9-digit number when you “check order status”.
Examples: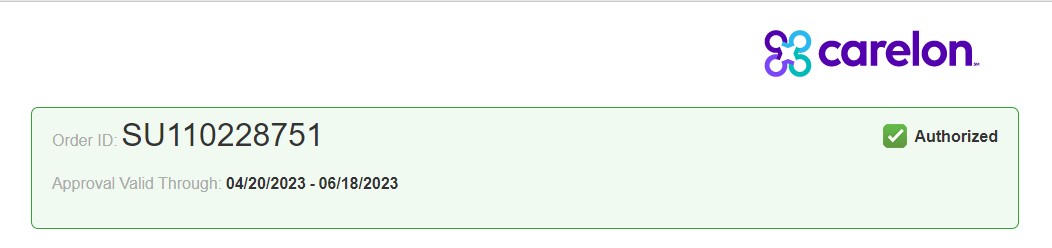
Tips for maintaining a smooth provider portal experience:
- Reboot daily – most programs have releases where new or existing functionality is updated; rebooting ensures that those most recent updates are reflected in your computer.
- Clear cookies and cache – periodically clearing your cookies and cache can keep your computer “clean” and promote efficiency. If you don’t know how, contact your IT department.
- Use the right browser – Use Google Chrome for optimal use of the provider portal. Please note that Internet Explorer (IE) has been retired.
Peer-to-peer requests / Specialty-matched provider consultations:
Requests that do not meet medical necessity criteria: When an order request cannot be approved immediately, you will have the option of discussing your case with one of our clinical experts. A peer-to-peer discussion with one of our Carelon clinician reviewers is always offered before any adverse determination is made. No adverse determination is made until the case has been reviewed by a clinician reviewer at Carelon.
It is important that when the Carelon clinician reviewer informs your office (always via phone or fax), that the case pends for peer-to-peer conversation, your ordering physician calls Carelon as soon as possible to discuss it with a Carelon clinician reviewer. Until we receive a phone call back, the case will continue to pend until it is due to close in accordance with health plan requirements. Urgent requests will pend for up to 72 hours after initial receipt of the case. At the time of required case closure, if the clinical information requested is not provided and/or peer-to-peer did not take place, the case will be denied. Denial letter will be sent to the member and provider.
How will we know when a peer-to-peer is needed?
When a case pends for review, it will go to an “In Progress” status. Carelon will request the ordering provider requesting a call-back for peer-to-peer review, should it be required.
More Information – Where can I access additional information?
For assistance contact us by email or at 800-252-2021.